The story so far:
With a population of 146 crore, India’s health challenges are growing too. It already faces an avalanche of non-communicable diseases, resurgent infectious diseases, climate change-related issues, concerns relating to quality control in the burgeoning pharmaceutical industry, and above all, funding for health care. As India gears up for health emergencies, it needs to prioritise and realign areas of care and attention to ensure health for all.
Why is there a funding deficit?
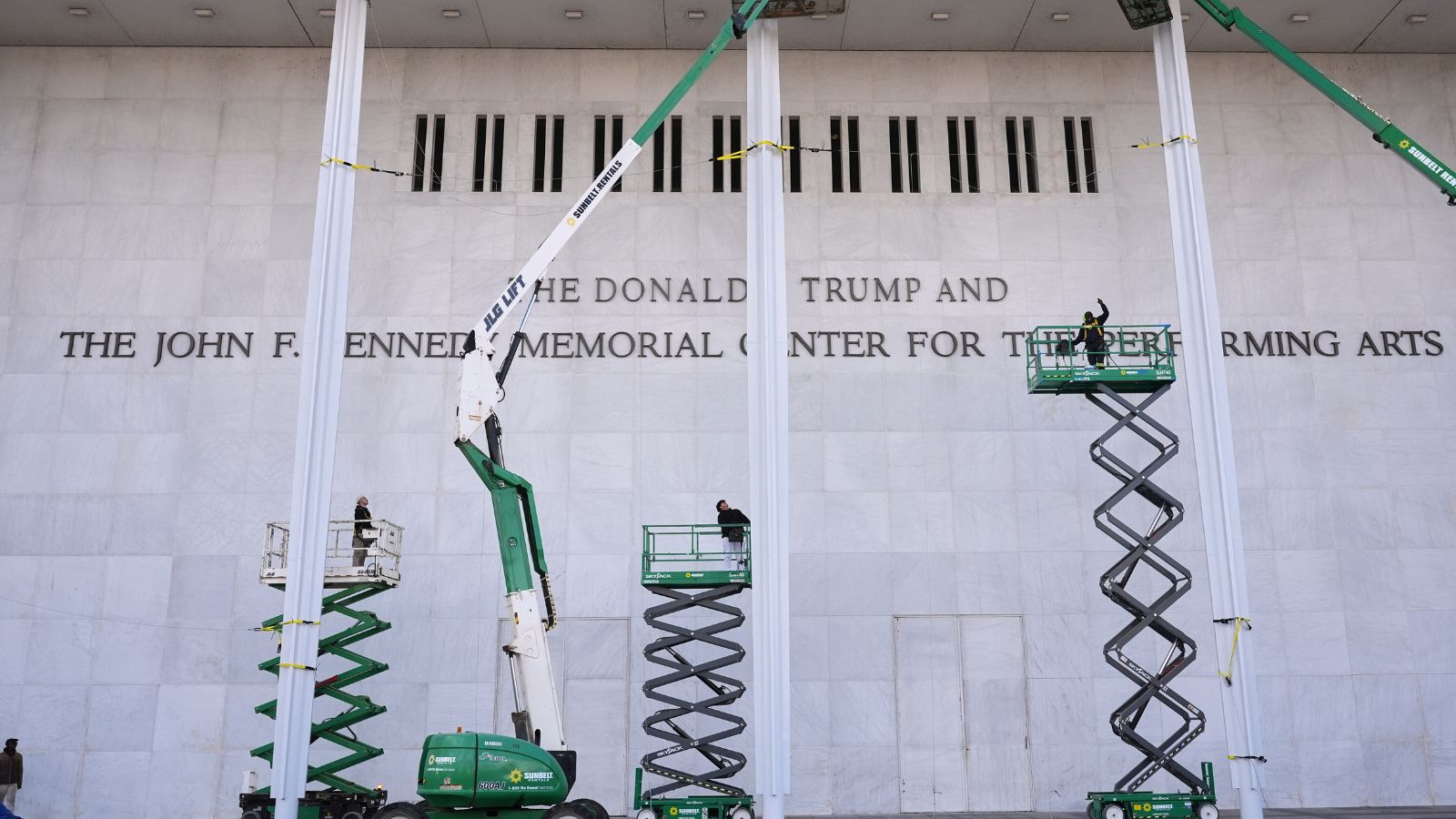
Early in 2025, Donald Trump’s presidency brought with it the withdrawal of the United States from the World Health Organization (WHO) and consequent withdrawal of funds for various health and development projects. The move affected India too — a beneficiary of the PEPFAR (U.S. President’s Emergency Plan for AIDS Relief) and USAID — as funds suddenly dried up for certain key health intervention projects in the fields of HIV/AIDS, population services and maternal and child health. The government said USAID committed $97 million in funds for seven projects, only part of a total budget of approximately $750 million allocated across all projects.
The Union and State governments have had to make good this funding deficit.
What about budgetary allocation?
India’s health budget has remained below 2% of the GDP, while the clamour to increase funding grows louder each year. A sum of ₹99,859 crore was allocated for various health projects in the 2025-26 fiscal year, an 11% rise from the previous year’s, and it is yet to hit the sweet spot of over 2% of the GDP. In fact, the National Health Policy itself set a target of 2.5% of GDP. Unless this is achieved, it is unlikely that India can achieve the larger goal of health for all. The ‘health for all’ movement has been gaining momentum over the years. While the post-pandemic years have brought health closer to the people, in terms of diagnostic labs and the number of beds, a huge gulf remains between demand and supply in funding and infrastructure.
What are some of the pressing concerns?
The chronic inadequacy of funding leaves one wondering if the health system will be able to handle the resurgence of several infectious diseases effectively enough to bring down the deaths and improve morbidity. In addition, the country now faces abysmal air quality issues, particularly in winter in northern cities. This has led to quality of life plunging dramatically in the general population, besides further crippling children, senior citizens and people who have pre-existing respiratory issues. Unless India takes a leaf from the China playbook and finds solutions to remedy air quality like in Beijing, further deterioration is assured.
Why did India miss the TB elimination goal?
India advanced the global target for achieving the elimination of tuberculosis by two years and reassigned 2025 as the year it would eliminate tuberculosis. However, that remains a pipe dream, though several advancements have been made over the years, particularly in terms of diagnosis, and more recently, drug regimens too. There are now sophisticated home-grown molecular tests such as TrueNat. The deployment of these machines across the country has not only enabled the speedy detection of the mycobacterium infection, but also drug resistance. However, the growing number of cases of multidrug-resistant TB and extensively drug resistant TB continues to be a cause for worry. Detection rates across the country are inconsistent and will need some work.
Why is antimicrobial resistance a cause for worry?
The larger issue of antimicrobial resistance (AMR) is of immediate concern in India. The WHO’s recent GLASS report noted that one in three people who had bacterial infections in India bore resistant organisms, against one in six globally. For India, the report flagged high resistance rates to major antibiotics, especially in serious infections such as those caused by E.coli, Klebsiella pneumoniae, and Staphylococcus aureus, particularly in hospital ICUs. The challenging factors that aggravate AMR are widespread over-the-counter antibiotic access, self-medication, incomplete courses, environmental contamination (from pharmaceutical manufacturing and hospital waste), and uneven enforcement of regulations. Notably, Kerala is the only State where stewardship in AMR has led to an actual lowering of AMR levels in the community; others need to catch up, even as they roll out the second iteration of the National Plan of Action on Antimicrobial Resistance introduced this year.
Why does India need to address its pharma quality issues?
The most pressing issue of the year was reserved for the last quarter. In all, 25 children died in Madhya Pradesh after consuming prescription cough syrup. A lab analysis revealed that the cough syrup, manufactured in Tamil Nadu, contained an industrial chemical, diethylene glycol, known to cause kidney and liver failure. While regulatory action was stepped up after the deaths of the children, many questions remain. Did the quality control mechanism embedded into the system fail? Are there other cases where poor quality, even poisonous drugs, have managed to skip past the regulator?
India, which is on a Make-in-India trajectory, will scarcely move ahead unless it gets a hold of quality, before it realises its ‘pharmacy of the world’ goal. The sad fact is that India’s cough syrups have always tussled with quality issues, with 70 children dying in The Gambia, Africa, after using cough syrups, four of them manufactured in India. Subsequent probes have revealed certain quality issues; that they continue to strike periodically, taking lives and reducing the quality of life of patients, is a statement on the pharma quality regulatory framework of the country.
The coming year will hopefully see India wrestle with contentious issues in the health care sector and overcome at least some of the glitches that threaten mortality and morbidity.


 14 hours ago
4
14 hours ago
4






















 English (US) ·
English (US) ·  French (CA) ·
French (CA) ·  French (FR) ·
French (FR) ·